What is PVD?
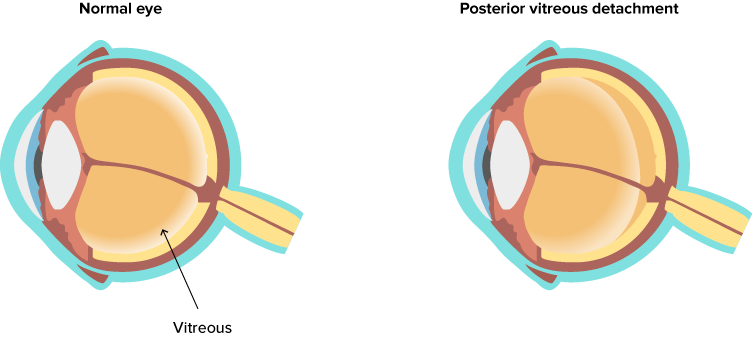
Posterior Vitreous Detachment (PVD) is a common eye condition.
The vitreous is the clear, jelly-like substance in your eye, which provides shape and nutrients to your eye. Light passes through the ‘vitreous gel’ to the retina at the back of the eye. A vitreous detachment occurs when the vitreous jelly comes away from the retina.
How do I get a PVD?
As you get older the various structures that make up your eye change. The vitreous part of the eye becomes more watery and less ‘jelly-like’ and isn’t able to keep to its original shape. This means that the vitreous is more likely to move away from the retina.
Trauma can also cause a PVD; anything from a boxer’s punch, or even in some cases from vigorous nose blowing. PVD can also occur after cataract surgery.
Who can get PVD?
It affects about 75% of people over the age of 65. Although less common for people in their 40s and 50s, the condition is not rare. Some research has found that the condition is more common among women. PVD is not a sign of disease or eye health problems. For most of us, PVD happens naturally as we get older.
PVD is rare for people with emmetropia (no distance vision correction needed) or those under the age of 40, but it increases with age to 86% for those in their 90s.
People with myopia (nearsightedness) are at a higher risk of PVD at any age.
Will PVD affect my vision?
PVD does not directly threaten vision, but there are some common symptoms;
- Floaters – dots, circles, lines or clouds, that move around in your vision
- Little flashes of light – as the vitreous pulls on the retina, it stimulates it to cause the sensation of a flash of light
- Cobweb effect across your vision
Some people get all three symptoms whilst others may only get one or two.
Importantly these same symptoms can be an indication of more serious problems such as a retinal tear, which needs urgent attention.
What to do if you suspect a PVD
The only way to tell if you have a PVD is to have your eyes examined by an optometrist. If you suddenly experience any of the following symptoms, you should have your eyes examined as soon as possible, preferably the same day, or at least within 24 hours.
- A sudden appearance of floaters, or an increase in their size and number
- Flashes of light and/or a change/increase in the flashing lights you experience
- Blurring of vision
- A dark ’curtain’ moving up/down or across your vision (this may mean that the retina has already partially detached)
It is important to remember, that in most cases these symptoms are caused by PVD alone, which rarely causes any long-term issues with your vision.
However, it is always advisable to have your eye(s) examined to confirm the diagnosis and to rule out retinal detachment or tears.
Treating PVD
Around 10% of PVDs develop into a retinal tear. And 40% of retinal tears can develop into a retinal detachment if left untreated.
For PVD alone treatment is not required – unless there are associated retinal tears. In PVD, the vitreous will continue to age and liquefy and the floaters should become less and less noticeable. Eventually, all symptoms will completely disappear. Continuous care and monitoring PVDs is the most effective means of preventing them from developing into retinal tears and detachments.
Should I avoid any activities after being diagnosed with PVD?
Most people with PVD have no restrictions on their activities.
There is no evidence to suggest any of these activities will cause problems with your PVD:
- Heavy lifting
- Strenuous exercise
- Contact sports
- Yoga / Pilates
You may find that during these activities your floaters are more noticeable. This is due to the movement during the activity rather than a change in your eye.
Some people take the personal decision to avoid certain activities when their PVD symptoms are quite intense, especially for a newly diagnosed PVD, they may choose to wait until the symptoms have calmed down.
You can carry on with all daily activities quite happily, and there is no evidence to suggest that flying in an aeroplane will harm your PVD or make it worse.
This advice might change if you have another condition, or depending on your eye health in general.
Your optometrist is the best person to give advice on any activity you should avoid.
Our fully qualified optometrists and eye management team are on hand to offer you support and continuous care with the management of PVD. We advise a thorough eye examination, including a retinal scan, to rule out any further problems.

